WHAT IS HOMEOSTASIS ?
- Homeostasis is a key concept in understanding how our body works. It means keeping things constant and comes from two Greek words: ‘homeo,’ meaning ‘similar,’ and ‘stasis,’ meaning ‘stable.’ A more formal definition of homeostasis is a characteristic of a system that regulates its internal environment and tends to maintain a stable, relatively constant condition of properties.Homeostasis is happening constantly in our bodies. We eat, sweat, drink, dance, eat some more, have salty fries, and yet our body composition remains almost the same. If someone were to draw your blood on ten different days of a month, the level of glucose, sodium, red blood cells and other blood components would be pretty much constant, regardless of your behavior (assuming fasting before drawing blood, of course).No matter how much water you drink, your body doesn’t swell up like a balloon if you drink tons, and it doesn’t shrivel like a raisin if you drink very little. Have you ever wondered about this? Somehow, our bodies know how much fluid we need to keep, and then maintain a constant level regardless of how much water we drink.
ORGANS INVOLVED IN HOMEOSTASIS
STRUCTURE OF KIDNEY AND NEPHRON
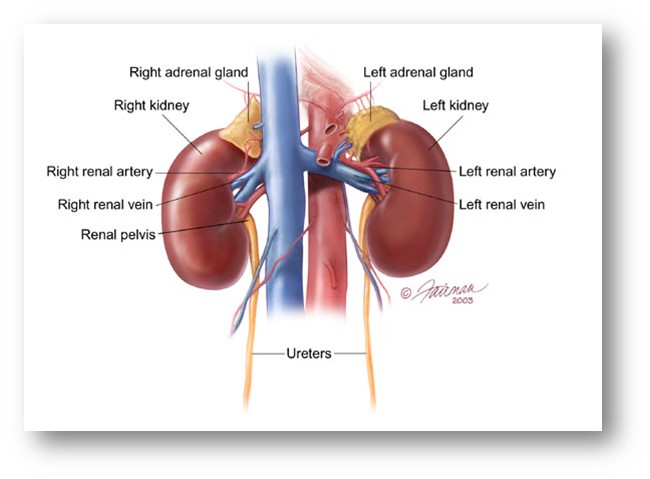
- The human kidney is a dark-red, bean-shaped organ about 10 cm long, 6 cm wide and 2.5 cm thick, with a weight of about 250 g. The pair of kidneys is attached to either side of the backbone, just behind the stomach and the liver.
- The outer surface of the kidney is covered by the renal capsule.
- The kidneys are attached by 3 tubes:
- The renal artery, which carries blood from the aorta to the kidney
- The renal vein, which carries blood from the kidney to inferior vena cava.
- A ureter, which carries urine to the bladder
4. The ureter divides into several branches, the ends of which envelop kidney tissues called renal pyramid (medulla pyramid). An adult kidney typically contains 8-15 renal pyramids. Renal pyramid made up the internal core, medulla of the kidney. The medulla is surrounded by the cortex.
5. Several minor calyces merge to form larger spaces called major calyces. Urine from the renal pyramids is collcted by minor calyces, drained into the major calyses, and then to renal pelvis, and finally transports into the ureter
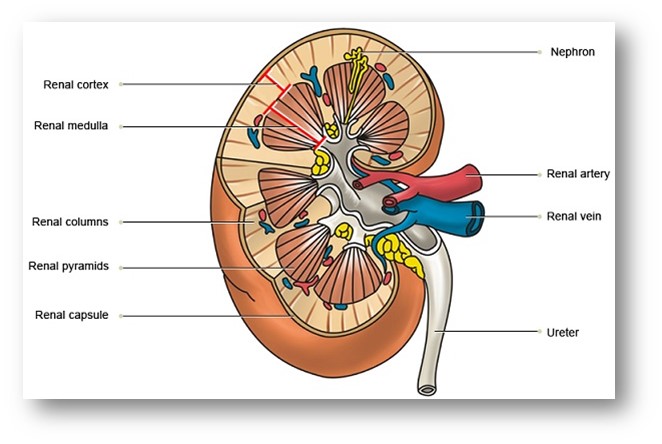
6. The gromerulli, Bowman’s capsule and the convulated portions of the kidney tubule are located in the cortex, whereas the straight portions of the tubules, loop of Henle and the urine-collecting ducts are located in the medulla.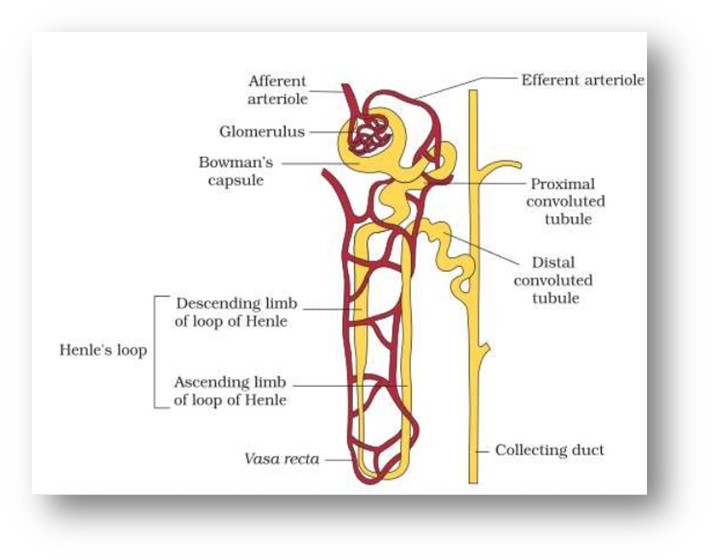
7. Each kidney contains about million tiny filtration units called nephrons. A nephron consists of a twisted hoolow tube, closed at one end and open at the other surrounded by a network of associated blood vessels.
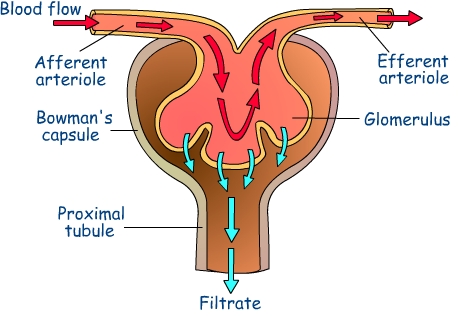
8. The renal artery enters the kidney and branches to form a series of arterioles, and these distribute blood to each nephron as a spherical cluster of capillaries, called the glomerulus.
9. All of the gromeruli are located in the cortex. Filtration of blood takes place here.
10. The blood leaving the gromerulus flow through anather capillary network surroundings the tubular portion of the nephron called vasa recta. The blood vessels then converge to form a system of veins that merge to form the large renal vein through which blood leaves the kidney.
11. The closed end of the kidney tubule is greatly expended to form a double walled funnel or capsule, called Bowman’s capsule. The 2 walls of Bowman’s capsule consists of a single layer of flattened epithelial cells each, and are separated from one another by a fluid-filled space. The cup-like portion of the capsule is almost completely surrounds the coiled ball of gromerular capillaries.
12. Leading from the Bowman’s capsule is a tubule, about 60µm in outer diameter, whose lumen is continues with capsule space. The first part of the tubule is highly coiled and is known as the proximal convulated tubule.
13. It leads to a U-shaped loop of Henle which then continues to another coiled section, the distal convulated tubule.
14. This portion opens into a collecting duct, along with those from several other nephrons. The ducts collect at the pelvis of the kidney, emptying their contents into the ureter which conveys the urine to the bladder for temporary storage.
FUNCTION OF KIDNEY: URINE FORMATION
1.Ultrafiltration
2. First proximal convulated tubule – Reabsorbtion
- All glucose, all amino acids and 85% of mineral ions are reabsorbed by active transport from the filtrate to the tissue fluid. They then diffuse into the blood capillaries.
- Small proteins are reabsorbed by pinocytosis, digested, and the amino acids diffuse into theblood.
- 80%of the water is reabsorbed to the blood by osmosis
- Surprisingly, some urea is reabsorbed to the blood by diffusion. Urea is a small, uncharged molecule, so it can pass through membranes by lipid diffusion and there isn’t much the kidney can do about it. Since this is a passive process, urea diffuses down its concentration gradient until the concentrations of urea in the filtrate and blood are equal. So in each pass through the kidneys half the urea is removed from the blood and half remains in the blood.
3. Loop of Henlé – Formation of a Salt Bath

4.Distal Convoluted tubule – Homeostasis and Secretion

STRUCTURE OF LIVER AND ITS FUNCTION

- Regulation of glucose or carbohydrates metabolism : Glucose that is removed from the blood is converted into glycogen for storage, or oxidized into CO2 and water with the release of energy. if there is considerable excess, the glucose can also be converted into lipids.
- Regulation of lipids : Lipids that are removed by the liver cells from the blood will either be broken down or be modified for storage in the fat depots.
- Regulation of amino acids and proteins

-
Detoxification : The liver cells absorb many poisons substances and detoxify them through chemical changes.
- Production of heat : The liver cells have a high metabolic rate along with its large size, thus making it an ideal source of heat. the excellent blood supply helps in the distribution of heat produced.
- Production of bile : Liver cells synthesises bile, which is stored in the gall bladder.
- Formation of cholesterol : Hepatocytes can synthesise cholesterol, which is an important constituent of plasma membranes. excess cholesterol is excreted in the bile. elimination of excess cholesterol is an important function of the liver.

-
Elimination of sex hormones : Some are modified chemically by the liver cells, some are sent to the kidney for renal excretion, and some are expelled in the bile.
- Formation of red blood cells : The liver is responsible for formation of red blood cells in the foetus. the bone marrow takes over this role later on. the liver stores vitamin B12, a porphyrin with cobalt in the center, which is required for the formation of red blood cells in the bone marrow.
- Elimination of haemoglobin : The old red blood cells are destroyed by phagocytic cells lining the blood vessels of the liver, spleen and bone marrow. haemoglobin is converted into the green pigment bilirubin, which is then reduced to the brown pigment, biliverdin. this is eliminated in the bile, giving it its characteristic colour.
- Storing blood : The veins in the liver have the ability to expand and contact gently. this allows the liver to store blood and serve as a blood reservoir.

- Synthesis of plasma proteins : These include fibrinogen, the protein responsible for the clotting of blood. the other plasma rotein sysnthesised in the liver and released into the circulation are albumins, globulins, heparin and clotting factors.
- Storage of vitamins and and minerals : Vitamins A, B12, D, E , K and a number of minerals such as potassim, iron and copper are stored in the liver.