WHAT IS GOUT?
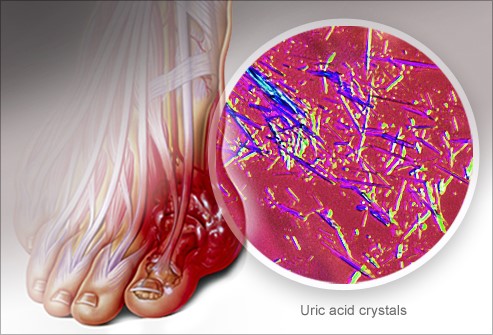
Gout usually develops after a number of years of buildup of uric acid crystals in the joints and surrounding tissues. A gout attack usually starts during the night with moderate pain that grows worse.
A gout attack typically causes pain, swelling, redness, and warmth (inflammation) in a single joint, most often the big toe. Then symptoms gradually go away.
- Most gout attacks stop after about a week.
- Mild attacks may stop after several hours or last for 1 to 2 days. These attacks are often misdiagnosed as tendinitis or a sprain.
- Severe attacks may last up to several weeks, with soreness lasting for up to 1 month.
- Many people have a second attack of gout within 6 months to 2 years after their first attack. But there may be intervals of many years between attacks. If gout is untreated, the frequency of attacks usually increases with time.
There are three stages of gout. Many people never experience the third stage.
- In the first stage, you have high uric acid levels in your blood, but no symptoms. The uric acid levels may stay the same, and you may never have symptoms. Some people may have kidney stones before having their first attack of gout.
- In the second stage, uric acid crystals begin to form, usually in the big toe. You begin to have gout attacks. After an attack, the affected joint feels normal. The time between attacks may grow shorter. Your later attacks may be more severe, last longer, and involve more than one joint.
- In the third stage, symptoms may never go away. They may affect more than one joint. Gritty nodules called tophi may form under your skin.
Without treatment, the tophi may form in the cartilage of the external ear or the tissues around the joint (bursae, ligaments, and tendons).
This can cause pain, swelling, redness, and warmth (inflammation). Progressive crippling and destruction of cartilage and bone is possible.
This stage of gout is uncommon because of advances in the early treatment of gout.
Articles-“Gout Flares Tied to Foods High in Purines”

FRIDAY, June 1, 2012 (MedPage Today) — Patients with gout who consumed high levels of purine-rich foods — including meats, organ meats, seafood, lentils, spinach, mushrooms, yeast, and beer — over a 2-day period increased their risk of flare almost five-fold, a case-crossover study showed.
Compared with individuals in the lowest quintile for 2-day purine consumption, those in the highest quintile had an odds ratio for recurrent gout attacks of 4.76, according to Yuqing Zhang, ScD, of Boston University, and colleagues.
It has been widely believed that habitually eating a high-purine diet can lead to increased flares of gout in susceptible individuals, but the effects of a short-term increase in consumption of foods such as organ meat and certain fish have not been fully examined.
“Clarifying this link and quantifying its magnitude would help gout patients make informed decisions about food items that should be limited or avoided,” Zhang and colleagues wrote.
Accordingly, they conducted an online study that included 633 participants with physician-diagnosed gout who provided information on demographics, medical history, and risk factors.
Participants also were queried in detail about food intake in the 2 days before a recent attack, as well as their symptoms and medication use.
Patients were their own controls, additionally providing information about dietary consumption during 2-day control periods at baseline and at months 3, 6, 9, and 12.
Average age of the participants was 54, and most were white men.
Allopurinol was used at some point during the year of follow-up by 45 percent, colchicine by 25 percent, nonsteroidal anti-inflammatory drugs (NSAIDs) by 54 percent, and diuretics by 29 percent.
During that year, there were 1,247 gout attacks, more than 90 percent of which involved a lower extremity.
Treatments for the acute flares included colchicine, corticosteroids, and NSAIDs.
During the 2-day control periods, median purine intake was 0.06 oz. for men, which would be equivalent to about 3.1 lbs. of beef or 6.4 lbs. of spinach. But during the 2 days before a gout flare, men consumed an average of 0.07 oz. of purines, which would have been about 3.8 lbs. of beef or 7.9 lbs. of spinach.
For women, the median purine intake during control periods was 0.05 oz. — about 2.6 lbs. of beef or 5.3 lbs. of spinach. Before flaring, women consumed 0.06 oz. of purines, which would be about 3.1 lbs. of beef or 6.4 lbs. of spinach.
The researchers also found that purine intake from animal sources was five times higher than from plant-based foods, at 0.03 oz. versus 0.006 oz. over a 2-day period.
“Our findings support the notion that plant-derived foods should be the preferred sources of protein for gout patients, given that plant food items (especially nuts and legumes) are excellent sources of protein, fiber, vitamins, and minerals, and studies have found their benefits against the risk of weight gain, coronary heart disease, sudden cardiac deaths, and type 2 diabetes,” Zhang and colleagues observed.
The study had certain limitations, including the lack of information on individual participants’ serum urate levels, and the possibility of recall bias regarding dietary intake.
In addition, the study did not consider the longer-term effects of high purine intake.
Nonetheless, these findings lend support to an anti-gout strategy of reducing purine consumption, particularly from animal sources, the researchers concluded.
WHAT IS HIGH BLOOD PRESSURE?
High blood pressure is a common disease in which blood flows through blood vessels (arteries) at higher than normal pressures.

Measuring Blood Pressure
Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps blood. High blood pressure, sometimes called hypertension, happens when this force is too high.
| 118/76 mmHg People read “118 over 76” millimeters of mercury. |
Articles-‘Why It’s Getting Harder To Decide When To Treat High Blood Pressure”
by Harlan Krumholz NPR | April 14, 2016 12:04 p.m.

Are you ready for some more uncertainty about blood pressure treatment?
Decisions about blood pressure have gotten more difficult over the last couple of years as experts in the U.S. have failed to reach consensus on recommendations about when drug therapy should be started. Now there’s new evidence that could make the decisions even more challenging.
Let’s review first where there is agreement. Around the world, high blood pressure causes a lot of harm. Your risk of health problems — such as heart disease, stroke, and kidney disease — increases with higher blood pressure.
Your lifestyle can influence your blood pressure. A healthful diet, at least moderate physical activity and weight control can bring down your blood pressure. Those are good habits for everyone, in fact.
Medicines can help reduce the risk for people with higher blood pressure, say 150 millimeters of mercury and above for systolic pressure, the top number. Too many people have untreated and uncontrolled marked elevations of blood pressure and many devastating health problems could be prevented if we could help people get proper treatment.
What about medicines for people whose blood pressure is high but less than 150? Most doctors agree that people younger than 60 would do well to keep their blood pressure less than 140. The consensus is that the benefit of drugs for those who didn’t respond to lifestyle changes exceeds the risks of treatment.
Some believe that for older patients, who may be more sensitive to medications, the recommendations should be more permissive and not push for treatment that brings blood pressure below 140. Then there’s the SPRINT trial, whose results were released last November and suggested that people without diabetes, even older people, would benefit by seeking to get their blood pressure down to around 120.
Another study, called HOPE-3 for short, added important evidence about the treatment of blood pressure that will further unsettle the field. The findings were published April 2 by in The New England Journal of Medicine.
So what did HOPE-3 find? The blood pressure medications worked. Study participants in the group that got blood pressure medicine had their systolic blood pressure lowered about 6 points more than those in the placebo group. However, after almost six years of follow-up, the investigators determined that lower blood pressure didn’t translate into lower risk. The risks of death from cardiovascular causes, heart attacks, strokes and other problems weren’t different between the groups.
The investigators explored the data further and found some evidence that the group in the highest third of blood pressure at the start (an average top number of 154) seemed to have a lower risk, while the group in the lowest third at the start (average of 122) seemed to do worse. These analyses were planned at the outset of the study, so we tend to give them a bit more weight.
So what happened?
HOPE-3 used common antihypertensive medications, an angiotensin receptor blocker called candesartan and a diuretic called hydrochlorothiazide. Could the results be explained by something about these medications?
Participants in the study had an average age of 65 years, about half were women, a quarter were smokers and almost all were overweight. Was there something special about them?
Or could it be that pushing blood pressure to ever-lower levels, even in a group at modest risk of heart disease and stroke, is just not producing benefit?
We don’t know for sure.
The field is waiting eagerly for the next version of national guidelines about blood pressure. A group of experts in the field will look at all the evidence and give its opinion about whom to treat and when.
But how useful will general guidelines be for individual patients, given the conflicting evidence? How confidently will the experts be able to recommend strategies for people in the middle range of blood pressure.
The ultimate decision about treatment for each person should be informed by the fact that a definitive benefit hasn’t been consistently shown for lowering blood pressure below 140 in people without known disease (we call this primary prevention). The results of the HOPE-3 indicate that the lower your blood pressure is, the less likely you are to benefit from starting drug therapy.
As always, if your blood pressure is in the range where there is controversy and you want to lower your blood pressure, your best first move is to adopt a healthful lifestyle and see what happens – and, of course, talk with your physician. Meanwhile, experts will be poring over the recent studies to try to reconcile the disparate results.
In medicine, we like it when the latest data bring clarity to personal decisions about treatments. But the reality is that studies often go in different directions and leave us even more uncertain about what to do next. That uncertainty, though, is still important information as you consider your options.
We need to move faster to get the knowledge that is attuned to our personal characteristics and that can guide our decisions about the blood pressure number that’s best and also the drug that would work best for each of us, if we need one. This is the hope of President Obama’s Precision Medicine Initiative. Given the mixed evidence we have, this new era of knowledge cannot come fast enough.
Harlan Krumholz is a cardiologist and the Harold H. Hines Jr. Professor of Medicine at Yale School of Medicine. He directs the Yale-New Haven Hospital Center for Outcomes Research and Evaluation and is a co-director of the Robert Wood Johnson Foundation Clinical Scholars Program.
WHAT IS DIABETES?
- Diabetesis a chronic condition associated with abnormally high levels of sugar (glucose) in the blood. Insulin produced by the pancreas lowers blood glucose. Absence or insufficient production of insulin, or an inability of the body to properly use insulin causes diabetes.
- The two types of diabetes are referred to as type 1 and type 2. Former names for these conditions were insulin-dependent and non-insulin-dependent diabetes, or juvenile onset and adult onset diabetes.

Articles–“Stop the Progress of Prediabetes”
By Madeline Vann, MPH| Medically reviewed by Cynthia Haines, MD
You can prevent this precursor to type 2 diabetes from developing into full-blown disease.

Don’t Miss This
Nearly 24 million American adults are living with diabetes, according to figures released last month by the International Diabetes Federation. But what may be even more alarming is that there are also about 79 million Americans with a condition known as prediabetes — and many aren’t aware of it.
Prediabetes means that while your blood sugar levels are higher than normal, that level isn’t high enough to warrant a diabetes diagnosis. However, a prediabetes diagnosis means it is time for action to prevent diabetes.
“In simple terms, there is a gap between what we call diabetes, which is a fasting blood sugar of 126 and above, and normal, which is less than 100 fasting,” explains Vivian Fonseca, MD, a professor of medicine and pharmacology and chief of endocrinology at Tulane University Health Sciences Center in New Orleans. “In between, you have impaired fasting glucose. If you do a glucose tolerance test, and you are in the gap, you have prediabetes. You are at risk for getting diabetes in the future and you are also at risk for heart disease.”
Research has also found that prediabetes may be more common in men than in women.
Type 2 Diabetes: Prevention
If you are told your blood sugar is abnormally high, you’ve just had a red flag waved in front of you. You’re being warned that unless you make some changes in your life today, your future will probably include a diabetes diagnosis.
“Walking 30 minutes a day and reducing weight by 5 percent can decrease the risk [of getting type 2 diabetes] by 60 percent over three years,” says Dr. Fonseca. While there are medications that have the same effect, lifestyle change is less expensive and has fewer side effects, Fonseca says.
Cutting your weight is crucial. “One of the links with obesity is that fat induces a mild low-grade inflammation throughout the body that contributes to heart disease and diabetes,” Fonseca explains. Without making any changes, you could develop type 2 diabetes within 10 years of first developing prediabetes.
Type 2 Diabetes: Who Should be Tested?
Prediabetes is a “silent” condition, says Fonseca. While some people may experience symptoms of diabetes such as fatigue or increased urination, most people’s blood sugar rises without any outward signs at all. This means you might not know you need to be tested for prediabetes — and even if you are screened, your doctor might not give you all the information you need to prevent it.
For these reasons, diabetes experts developed criteria for those who should be tested. The American Diabetic Association recommends that any adult age 45 or older should be tested for diabetes and prediabetes.
The ADA also recommends that any adult under age 45 who is overweight and has at least one of the following risk factors should be tested:
- Family history (especially parent or sibling with diabetes)
- Physically inactive lifestyle
- Native American, African-American, or Hispanic heritage
- Prior gestational diabetes diagnosis
- Birth of a baby over nine pounds in weight
- High blood pressure or treatment for high blood pressure
- Polycystic ovarian syndrome (PCOS) diagnosis
- Dark, velvety rash around the armpits or neck
- History of heart disease
- If your test reveals that you have prediabetes, you should be tested again in one to two years, depending on your doctor’s recommendations.
Type 2 Diabetes: Types of Tests
There are two tests used to screen for diabetes and prediabetes:
- Fasting plasma glucose: a test of your blood after you haven’t eaten for eight hours (usually overnight)
- Oral glucose tolerance test: a comparison of your blood taken first after eight hours without food (fasting) and then two hours later after you have consumed a sugary drink given to you by the lab technician.
If you fit the screening criteria listed above, make an appointment to get tested as soon as possible. It could be the first step toward preventing the development of type 2 diabetes.
iframe width=”420″ height=”315″ src=”https://www.youtube.com/embed/QeT1V8RmIbU” frameborder=”0″ allowfullscreen></iframe>
